Designing for Resilience, Not Just Efficiency
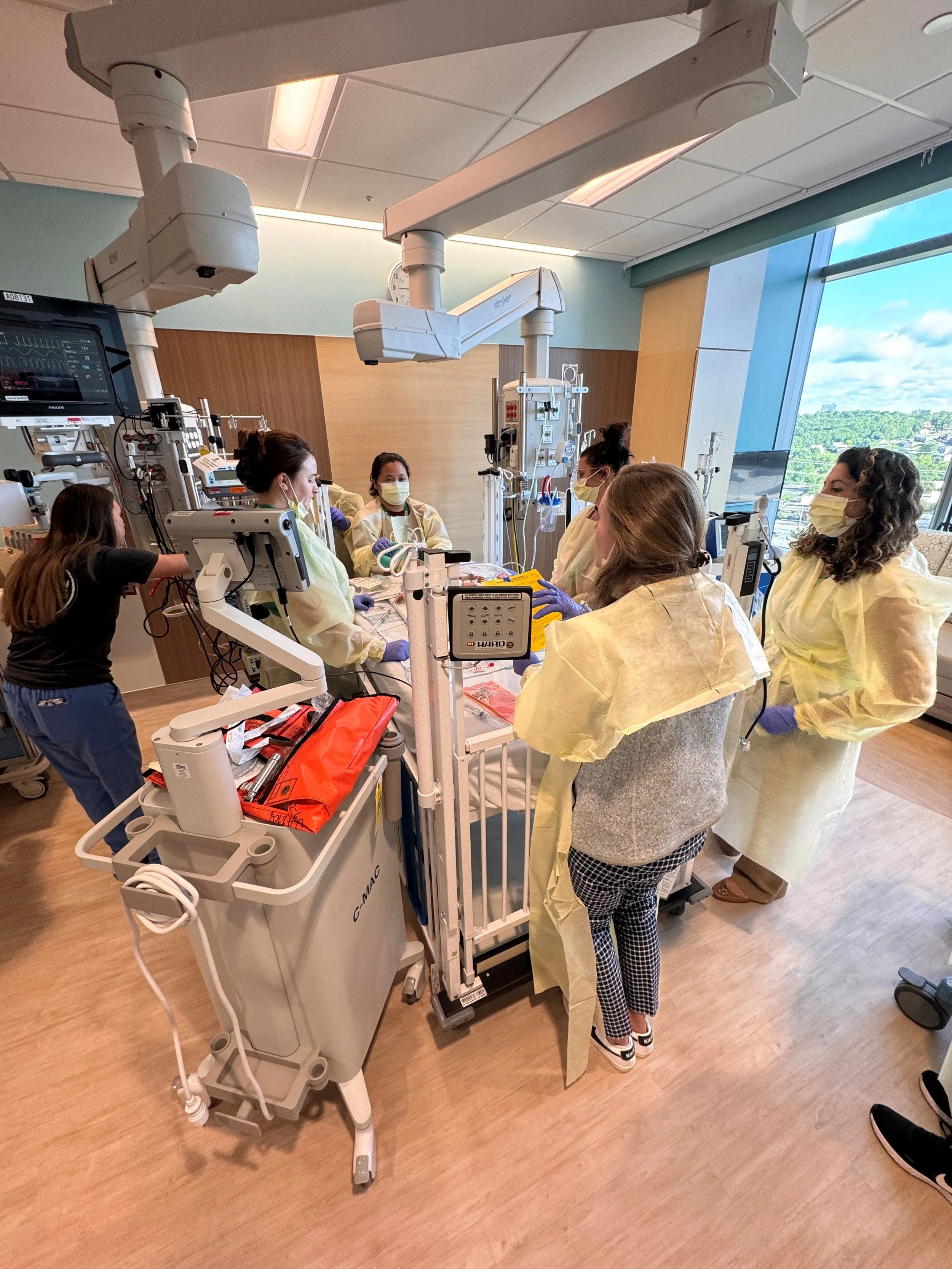
Care delivery is not linear. It is dynamic, interrupted, emotionally charged, and constantly evolving. While traditional design processes often envision ideal workflows, real-world practice is shaped by urgency, unpredictability, and the human response to complexity.
Human factors science encourages us to see errors not as isolated failures, but as opportunities to better understand how system design influences performance. Layout, visibility, acoustics, and spatial relationships shape how clinicians move, think, and communicate — affecting not only efficiency, but resilience, decision-making, and the ability to adapt in moments of pressure.
Safety-centered design does not seek to eliminate every misstep; rather, it focuses on building systems that anticipate disruption and support the unpredictability that is inevitable. This means creating environments that enhance situational awareness, reduce cognitive burden, and enable coordinated response when conditions rapidly shift.
A truly resilient environment acknowledges that clinicians are human. It designs intentionally for focus, clarity, teamwork, and adaptability when stakes are highest.
Without meaningful clinician engagement, design risks optimizing for theoretical scenarios rather than lived experience. Interdisciplinary co-design brings visibility to the subtle choreography of movement, communication, and improvisation that defines real care — allowing spaces to better support both what is planned and what is inevitably unplanned.
The CPR corridor scenario is not an exception; it is a powerful reminder that healthcare environments must be prepared not only for routine operations, but for the unpredictable realities of care delivery.